Making a Positive Difference.
The ERC’s website is dedicated to the memories of Ellen Johnson, Courtney Lee Crismore and Kristi An Rose.
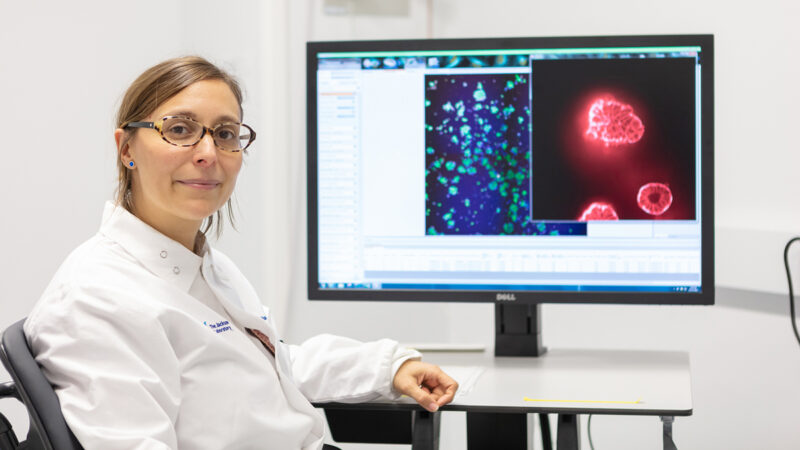
Endometriosis is a painful disease affecting an estimated 200 million individuals around the world. Characterized by the presence of endometrial-like tissue found elsewhere in the body, the disease causes chronic pain, inflammation, organ dysfunction and much, much more. As an inclusive organization striving to address the wide-ranging impact of the condition, including among teens and adolescents, gender diverse people and caregivers of those affected by endometriosis, we work on many national, international and regional initiatives through global collaborations and dedicated local groups. Endometriosis goes beyond age, race and socioeconomic status, affecting people from all backgrounds. Mistakenly stigmatized as merely “painful periods,” endometriosis is far more than just “killer cramps” – the far-reaching impact of the disease negatively impacts all of society, with healthcare cost burdens soaring into the billions. Endometriosis is also often mistaken for other diseases, and symptoms are frequently dismissed – leading to a ten year or longer delay in diagnosis. The ERC has worked tirelessly since 1997 to make a positive difference in the lives of all those living with endometriosis. The ERC is also pleased to be a partner of the EndoWhat? Coalition. Look around our site, and let us know how we can help you.
 March is Endometriosis Awareness Month
March is Endometriosis Awareness Month
We are very pleased to support EndoWhat? and Below the Belt, the leading endometriosis documentaries featuring knowledge straight from advocates. The ERC does not receive any proceeds from our collaborative efforts. Sales of these movies help fund EndoWhat’s critical educational efforts for school nurses and health care providers and other important national initiatives. Learn more below:
Could you have endometriosis?
Any of the following common symptoms (not a complete list) may be indicative:
- Chronic pelvic pain
- Pelvic pain that gets worse after sex or a pelvic exam
- Chronically heavy or long periods
- Bowel or urinary pain or disorders, often associated with periods
- Painful sexual activity and/or penetration
- Significant lower back or leg pain, sometimes worsening with menses
- Allergies, migraines or fatigue (may worsen with menses)
- Crippling menstrual pain
- Collapsed lung (thoracic endometriosi
Thank you to Commander Susan Pierce Richards, DNP, artist Angie Whitney and the Selah Fun Runners for their generous support of the ERC’s website design.

 March is Endometriosis Awareness Month
March is Endometriosis Awareness Month